Cervical Disc Bulge & Radiculopathy
Anatomy:
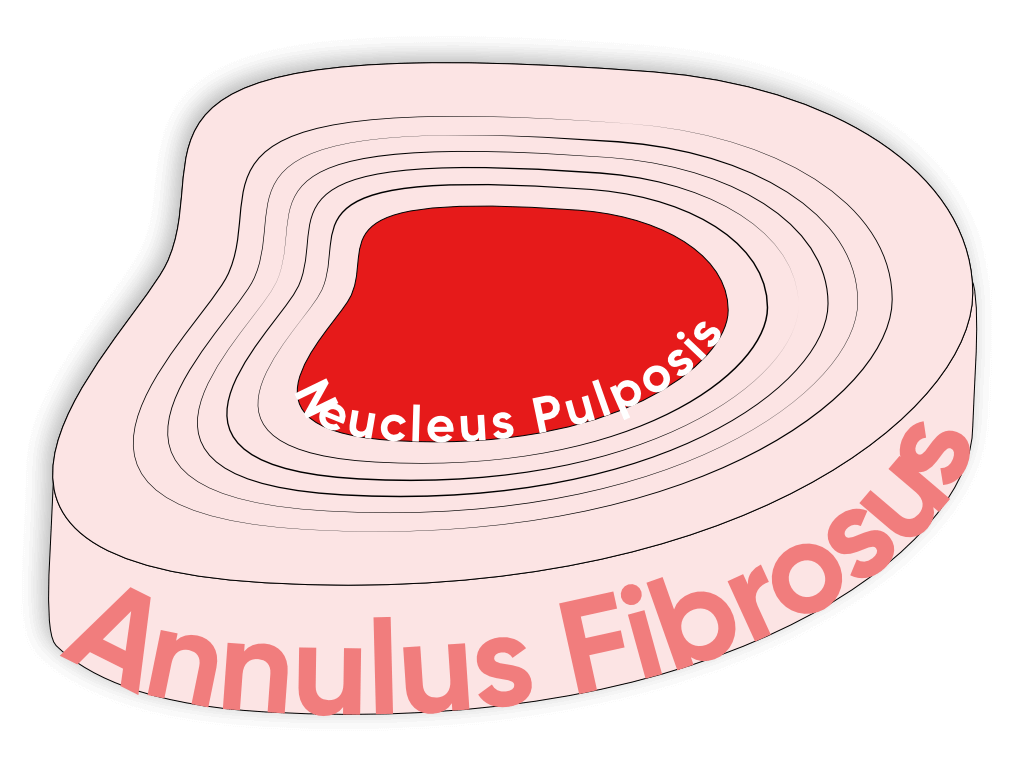
The Cervical Spine consists of seven vertebral bodies starting from the base of the skull, named C1 through to C7. For today’s topic we’re going to be focusing on the intervertebral disc (IVD) which sits in between each vertebrae (bony body) and acts as an impact cushion during activities which place load into the spine. The disc has a tough exterior called the Annulus Fibrosus (AF), and a gel-like centre called the Nucleus Pulposus (NP).
Intervertebral Disc Anatomy
When the AF is damaged, it allows the NP to be displaced. This can lead the IVD to compress and expand past the vertebral body, which is called a Disc Bulge. If the NP starts to compress upon the nerves or spinal cord, this is called a Disc Herniation. Either can cause pain and spinal dysfunction.
Anterior Longitudinal Ligament - helps prevent antero-lateral (forwards and to the side) disc herniation
Posterior Longitudinal Ligament - helps prevent postero-lateral (backwards and to the side) disc herniation
Brachial Plexus:
As mentioned previously in the Thoracic Outlet Syndrome (TOS) blog, the Brachial Plexus is composed of nerves branching from the lower cervical spinal cord. This is where the two conditions will overlap and find difficulty definitively placing a diagnosis on the patient's pain with symptoms alone. With TOS compressing the brachial plexus further toward the shoulder a cervical disc compression will be seen to impinge on the nerves closer at the neck, however ultimately compressing the same length of nerve.
The C5-C6 nerve root becomes part of the upper trunk of the brachial plexus and the C7 nerve root becomes part of the middle trunk of the brachial plexus
Disc herniation compressing the nerve root, or the beginning of the nerve that branches off the spinal cord (commonly nerve roots part of the Brachial Plexus) is called Cervical Radiculopathy. Characterised by pain down a one or multiple distribution areas associated with a particular level of nerve root, with muscular weakness and hyporeflexia (Reduced reflexes)
(Nikolaidis et al. 2010), (Sharrak, S, & Al Khalili, Y. 2021), (Dydyk, A.M, et al 2021)
Terms:
Education is the most common part of our job, ensuring when you leave the clinic as a patient you are not only educated in your condition but aware of misinformation that has made its way into the medical field.
For a disc related condition we commonly hear disc bulge, slipped disc and even “My neck is out”. Terminology that is harmful can be worse for the patient than the condition itself, causing anxiety and catastrophizing when symptoms appear. So lets clarify a few things and expand on the differences between particular disc conditions.
Disc herniation, disc protrusion, and disc bulge are often used interchangeably, these pathologies are not the same and have some key differences.
Herniation: A “localized or focal displacement of disc material beyond the limits of the intervertebral disc space.” This represents annular expansion extending beyond the disc space therefore a disc bulge is not a disc herniation, but rather a form of disc degeneration.
Disc herniation injuries can then be sub-categorised in regards to severity.
Protrusions - wide-based herniations in which the diameter at the base of the herniation is wider than the diameter of the herniation in the spinal canal.
Extrusions - narrow base, with a large herniation in the spinal canal
Sequestrations are herniations in which there is no continuity between the herniation and the remaining intervertebral disc
Image taken from Schroeder et al. 2016
To better understand what type of bulge, herniation or any other disc condition you have will require a high level investigation such as an MRI or CT scan, simply palpating or having your body tested is not a satisfactory way to diagnose specific severities of these conditions.
Loading:
This is the why part, but don’t get me wrong it is only a portion of it. By this I mean why has my disc bulged or herniated.
Intervertebral discs are subject to Axial loading or what we know as gravity! The load gravity and the weight of our body has on our discs is considerable however that is what they are designed for. Throughout the day this loading will decrease the height of the discs and then through off- loading overnight the height will return and be ready for the next day of axial loading.
Additional loads are predominantly flexion and also to some extent extension of the spine as well as lateral bending of which will load pressure on the opposing side of the disc to the direction you’re bending, for example “When I bend my head to the right I feel pain on my left side or down my arm, a common symptom of these conditions. (Schroeder et al. 2016)
Symptoms:
As mentioned above symptoms of a cervical radiculopathy will be similar to that of a Neurogenic TOS, most commonly nerve pain, numbness or tingling in the arm, hand or fingers depending on the level of compression.
Other major symptoms include sensory deficit most commonly in the elbow, decreased tendon reflexes and more importantly weakness of the muscles in the upper arm, forearm and hand.
Where the sensory deficits and neurological pain present in the limb will be directly related to the level of where that nerve root branches from the spinal cord as seen across in the image (Carleton-Bland, Wilby, 2018)
The presence or absence of neck pain should not be an indicator that a cervical disc condition or radiculopathy is present as localised neck pain will be present in a wide range of conditions.
(Verhagen, A.P. 2021)
Testing:
Physical examination will generally consist of seated and standing cervical posture, palpation, measuring the range of motion, especially in the directions mentioned above that will load the cervical discs.
When a diagnosis of cervical radiculopathy is suspected then measuring muscle strength, testing reflexes & sensation is important.
The choice of which of these physical examination procedures will be performed depends on the findings from the questions we ask at the start and throughout the session as the aim of physical examination is to confirm or rule out that initial working diagnosis.
When conducting any examination it is also important to clear the patient of any ‘Red Flags’ which are symptoms indicating quite serious pathology that will need to be further investigated. In the instance of the neck, injuries such as fractures, vertebral dislocation, injury to the spinal cord, infections or systemic diseases may be present.
(Verhagen, A.P. 2021)
Treatment strategies
Education & Advice : Understanding what is going on within your own body helps you make informed decisions towards your personal health and can help ease anxieties about your recovery.
Exercise Prescription : Based on presentation, the practitioner may incorporate either strength, endurance, and stabilising exercises or a combination of all which is inline with recommended guidelines.
Manual Therapy : Treatments such as remedial massage and mobilisation may provide an immediate influence on pain but are not demonstrated to provide long-term effects.
Thermal Therapies & Electrical Stimulation : May provide short term relief as the neck is recovering and improving.
(Eubanks, J.D. 2010)