Temporomandibular Disorder (TMD) and Myotherapy
What is Temporomandibular Disorder?
Temporomandibular joint and muscle disorders is commonly called ‘TMJ/TMD’, which encompasses a group of conditions that cause several complex symptoms, pain and dysfunction in the jaw joint and the muscles that control jaw movement.
For most people, pain in the jaw joint or muscles does not signal a serious problem. Generally, the discomfort felt from these conditions is often cyclic in nature. In some cases TMJ pain will go away with little or no treatment. However, some people can develop significant, long-term symptoms that can affect one or both TMJ’s muscles and surrounding tissues.
What is the Temporomandibular Joint?
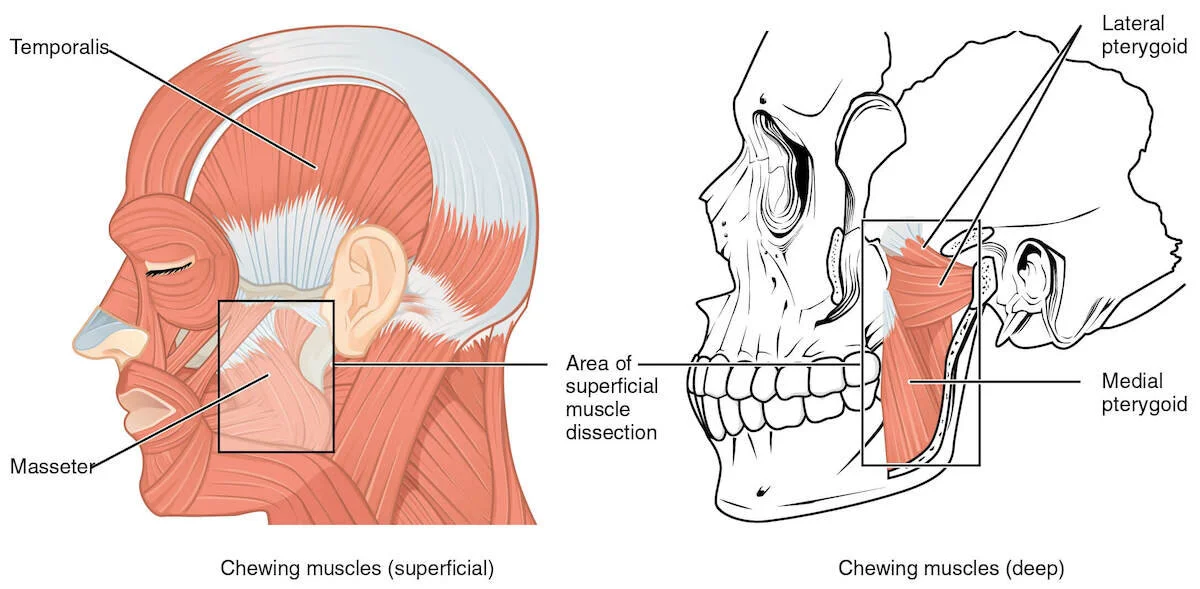
The temporomandibular joint (TMJ) connects the lower jaw (mandible) to the bone at the side of the head (temporal bone). If you place your fingers just in front of your ears and open your mouth, you can feel the joints move.
The TMJ is among the most complicated joints in the body as it can hinge and slide, allowing the jaw to move up and down; back and forward; and side to side. Therefore, it is an important part of your skull that helps you chew, swallow and talk. The main muscles that assist the jaw in these movements are the masseter, temporalis lateral pterygoid and medial pterygoid.
It is important not to overlook the various neck muscles that can contribute to TMD or create referred pain patterns to the head and face. The study “Characteristics of 511 patients with temporomandibular disorders referred for physical therapy”, found that that 69% of all TMD clients had a cervical or neck component, validating the consideration of treating the cervical spine or neck for the overall wellbeing of a patient suffering from TMD.
The management of TMD often involves multiple practitioners due to its complexity. Dentists are often the first contact with jaw pain, many of whom work hand in hand with Myotherapist’s or Physio’s to address contributing factors from the soft tissues.
Symptoms
Although no two patients pain and symptoms are the same, presentations can be simple to complex, below is a list containing some of the common TMD symptoms:
Headaches (tension or migraine)
Clicking, popping or grating sound in the jaw joints
Bruxism – Teeth grinding/clenching
Neck ache and back pain
Ear pain/stuffiness
Facial pain & muscle spasms
Pain & tenderness in the muscles of mastication (chewing) and the joint
Limited opening or locking of the jaw
Asymmetrical lateral shift of the TMJ
Uncomfortable ‘off’ bite/ Unexplained tooth pain
What causes TMD? Who and how?
TMD affects between 20–30% of the adult population where gender is a major predetermining factor of TMD, with up to 80% of people presenting for treatment being female, and typically between the ages of 20 and 40 years old.
When looking at the cause of the pain associated with TMD, it is rarely seen from factors such as degenerative joint disease or osteoarthritis, although direct trauma is a possible causative factor, a clear majority of people develop this condition slowly.
Common causes can include:
Stress: emotional and/or physical
Injuries to the jaw joint
Diseases such as rheumatoid arthritis, fibromyalgia or gout
Neck and upper back restriction, tight facial/mouth muscles/myofascial trigger points
Dental work
Poor posture
Bruxism: Clenching or grinding, which may be linked to stress
Parafunctional habits: nail-biting, frowning, chewing on pencils, etc.
How can a Myotherapist help with TMD?
Depending on the patients’ symptoms and level of pain, Myotherapist’s have a variety of different modalities to choose from when treating TMJ. Each technique and modality is designed to directly affect the TMJ to resort function and reducing pain.
Massage & trigger point therapy:
Massage and trigger point therapy should not be overlooked and is recognised by medical practitioners. Myofascial release and soft tissue massage target the muscle and fascial systems, promotes flexibility and mobility of the body’s connective tissues, helps reduce any inflammation, sensitivity and TMJ pain. Depending on the patient and symptoms the massage to the muscles of mastication can performed externally and intraorally (inside the mouth).
Dry needling:
Dry needling is not necessarily our initial treatment of choice for TMD, and to be clear there needs to be a muscular component to the diagnosis for dry needling to be effective. At least 70% of TMD cases there is a strong myofascial or muscle component. The study “Characteristics of 511 patients with temporomandibular disorders referred for physical therapy” validated that the largest diagnostic subset of TMD was myofascial pain or masticatory (chewing) muscle pain.
Dry needling causes favourable biochemical changes which assist in reducing pain. Dry needling has been shown to reduce abnormal Electromyography activity (the measurement of electrical activity of muscle during rest) and aberrant muscle contraction. Furthermore, benefits have been shown to occur locally and widespread within the muscular system. Muscles that are commonly targeted to treat TMD are the masseter, temporalis, SCM, suboccipitals and upper trapezius.
Muscle Energy Techniques (MET):
MET is an active technique and may be useful in engaging the nervous system to effect change in the TMJ. It involves the patient activating certain muscles or muscle groups in a specific direction against a precise resistance provided by the practitioner. By activating a muscular reflex these techniques gently encourage a return to the normal range of motion. A MET can assist to:
Relieve muscle spasm
Improve joint range of motion
Stretch tight muscle and fascia
Strengthen weak muscles
Muscle energy techniques are effective in TMD along many other conditions. The muscular spasm and joint restriction that is relieved will often be associated with a reduction in pain as well.
Exercise rehabilitation & how we can get you to help manage this condition?
Rehabilitation exercises are essential in the recovery and management of TMD, some exercises and management techniques you can perform at home could include:
General Rest Position
Place tongue behind the front teeth and allow your jaw to relax with teeth slightly apart. Your teeth should only touch momentarily when you swallow. Remember, if your teeth are touching, you’re clenching.
Retrusive Exercise
Curl your tongue upwards, placing the tip as far back on the roof of your mouth as possible, then slowly open and close your mouth.
Shoulder Retraction
Sitting or standing with an upright posture, retract and depress your shoulders while maintaining proper neck posture.
Neck Release
In an upright posture, laced hands behind your neck, then gently nod your head.
Calm Your Muscles, Your Mind & Manage Your Stress Levels
Tight, tense and tender muscles are one of the biggest contributors to TMD and the associated symptoms. It is important you gain a better understanding of what aggravates and alleviates your pain. Stress levels and mood must be managed as it is generally agreed that anxiety, depression, frustration and resentment may contribute to TMD through bruxism
Avoid Extra Pressure On Your Jaws
Avoid habits that will overuse your TMJ, such as sleeping on your stomach, resting your chin on your hand, holding the phone to your shoulder, biting nails, chewing gum etc.